Guidelines on how to safely deploy UV-C lighting to kill viruses
By Michael Litvin
 UV-C lighting, when correctly applied, will render the SARS-CoV-2 virus inactive and can be vital in containing the spread of COVID-19.1 Properly calculated dosages of direct UV-C illumination will deactivate the DNA of bacteria, viruses and other pathogens within the air and on surfaces to destroy their ability to multiply.1 The benefits of UV-C lighting over other methods of disinfection such as chemicals are numerous and include no dangerous residue, no harmful odors and negligible renewal costs. Yet current UV-C technology is not without its inherent risks, so how can these risks be mitigated for safe implementation?
UV-C lighting, when correctly applied, will render the SARS-CoV-2 virus inactive and can be vital in containing the spread of COVID-19.1 Properly calculated dosages of direct UV-C illumination will deactivate the DNA of bacteria, viruses and other pathogens within the air and on surfaces to destroy their ability to multiply.1 The benefits of UV-C lighting over other methods of disinfection such as chemicals are numerous and include no dangerous residue, no harmful odors and negligible renewal costs. Yet current UV-C technology is not without its inherent risks, so how can these risks be mitigated for safe implementation?
First, a few “UV ABCs.” Ultraviolet C is a form of electrical radiation that is present in sunlight and is fully absorbed by the Earth’s ozone layer prior to reaching the surface. Any instance of UV-C light on the surface is artificial and can be re-created via different lighting technologies such as mercury and LED-based lamps. UV-C light is divided on the UV Spectrum as 200-280 nanometers and precedes Ultraviolet B as 280-320 nanometers and Ultraviolet A as 320-400 nanometers The longer the wavelength of light, the deeper the penetration of the light into the skin. All three wavelengths possess carcinogenic2 and acute eye damage3 risks dependent on the degree of exposure.
Based on the risks, it is imperative that direct exposure to UV-C lighting be prevented. Therefore, whole room UV-C treatments should be automated to occur only during periods of non-occupancy. In order to prevent user error, lighting controls that possess automated scheduling features and remote activation are recommended over those that require manual user input. Occupancy-based sensors that immediately shut lights off upon sensing motion should be utilized. Care must be taken to ensure that the sensors do not falsely trigger, which would affect the efficacy of the UV-C treatment. Another point of concern is to ensure that sensor time delays are correctly programmed to ensure that the UV-C lights do not reactivate before an occupant leaves the treatment area.
Placement, wiring and configuration of the controls systems is crucial for proper application and should be done after consultation with lighting control experts. All automated control systems should maintain memory backup and resume normally scheduled operation when re-powered after an outage.
Further safety measures to avoid accidental exposure include affixing warning labels that specify treatment areas and operational hours placed in visible locations next to said areas. Locking the facility or rooms during treatment times is also effective. As long as the UV-C lights are not in direct view, light spillover is not a significant safety concern. Since UV-C radiation has a relatively short wavelength, it is absorbed by most surfaces and poorly reflected, leading to minimal spillover. Remote audio or visual alerts that deter people from entering the treatment area provide an additional layer of safety.
Regularly scheduled UV-C lighting treatments are best for continued whole-room air and surface disinfection. The amount of UV-C radiation that is received on surfaces depends on their distance from the UV-C emitter and whether the treatment area is partially or fully shadowed.4 Air flow, temperature, humidity and any objects between the source and pathogens, such as a virus encased in water, are additional factors that should be considered when calculating UV-C dosage criteria. Dosage levels, times and/or placement of the UV-C emitter(s) may have to be adjusted depending on the unique characteristics of the treatment area.
In order to ensure optimal lighting coverage, the placement and photometric properties of the UV-C lights must be taken into consideration. Overhead positioning from several UV-C light sources is recommended for shadow reduction as shown in Figure 1.
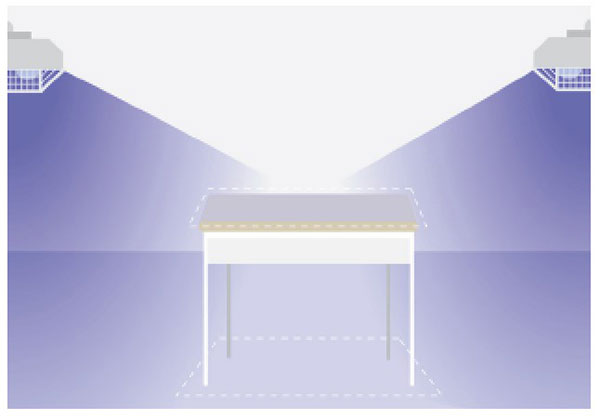
Treatment areas with objects that obstruct UV-C beam angles may require further spot-cleaning via portable and/or handheld UV-C light devices or in collaboration with other proven disinfecting means. A professionally calculated lighting layout and dosage schedule is the most efficient method to ensure that the UV-C lighting treatment fully disinfects the intended area without any blind spots.
What follows are some additional considerations to facilitate safe and effective cleaning:
Personnel Protection. Staff that work around active UV-C lighting systems and as such that are exposed for prolonged periods to UV-C radiation should wear protective equipment. UV-C goggles, specialized suits to cover exposed skin and other safety equipment can easily be found online.
Fading. Prolonged exposure to UV-C light will cause fading of colors on some materials. Although this is not a safety issue, preventative measures should be taken to shield surfaces and objects such as paintings, photos and fabrics where fading may be a concern.
Lamp Replacement. As with any light source, UV-C lamps will gradually lose effectiveness over their operational lifespan. Lamps should be replaced when their output falls below recommended treatment values and not necessarily replaced at end-of-lifespan as with traditional fluorescent lighting sources. End-users should be provided with a recommended lamp replacement date. Automated reminders and/or monitoring will further ensure that routine UV-C treatments are not missed on account of lamp failure. Lastly, routine cleaning of the UV-C light source is recommended in order to prevent a thin layer of dust or residue on the outside of the lamps negatively affecting ultraviolet output. This should be performed by the end user or service company in accordance with the manufacturer’s instructions.
Lamp Configuration. In order to prevent mix-ups with other types of lamps such as fluorescent and LED, UV-C light sources should employ unique lamp configurations that do not match the facility’s lighting infrastructure. Correspondingly, UV-C disinfection equipment should be designed to only accept UV-C replacement lamps in accordance with the manufacturer’s specifications.
Ozone. Ozone (03) is a hazardous gas that is created when the light emitted by 185-nanometer UV-C low-pressure mercury lamps interacts with oxygen. Inhalation of ozone can lead to a reduction in breathing capacity. Studies have shown that some subjects respond to ozone at concentrations as low as 0.37 parts per million (ppm).5 UV-C lamps operating exclusively at 254 nanometers will not produce significant amounts of ozone. Whereas some low-pressure mercury lamps produce noticeable amounts of ozone on account of emitting UV-C at both 254-nanometer and 185-nanometer wavelengths. As new manufacturing standards and requirements are still being adapted, ozone-producing lamps that emit at both wavelengths but are mislabeled as 254-nanometer lamps are currently making their way into the market. It is recommended that UV-C lamps are tested for ozone prior to implementation. Ozone emits a pungent odor which makes it very easy to notice. 03 meters to measure actual ppm concentrations are simple to use and relatively inexpensive.
When safely implemented, the benefits of a UV-C disinfection system greatly outweigh the risks. As a result, UV-C technology is becoming more commonly adapted for disinfection as safety measures become better understood and nationally recognized. New and increased disinfection protocols will affect everything from our work space6 to how we interact in a public setting. With the post-pandemic landscape on the horizon, UV-C technology has the potential to illuminate our way forward.

Sources
1 UV-C can effectively inactivate the SARS-CoV-2: Illuminating Engineering Society Photobiology Committee. Report CR-2-20-V1. “IES Committee Report: Germicidal Ultraviolet (GUV) – Frequently Asked Questions.” Illuminating Engineering Society, 15 April 2020, Available online: https://media.ies.org/docs/standards/IES-CR-2-20-V1-6d.pdf (Accessed 28 May 2020). Burhan K. SaifAddin, Abdullah S. Almogbel, Christian J. Zollner, Feng Wu, Bastien Bonef, Michael Iza, Shuji Nakamura, Steven P. DenBaars, James S. Speck. AlGaN Deep-Ultraviolet Light-Emitting Diodes Grown on SiC Substrates. ACS Photonics, 2020; Signify. “Signify and Boston University validate effectiveness of Signify’s UV-C light sources on inactivating the virus that causes COVID-19.” Available online: https://www.signify.com/en-us/our-company/news/press-releases/2020/20200616-signify-boston-universityvalidate-effectiveness-signify-uvc-light-sources-on-inactivating-virusthat-causes-covid19 (Accessed 17 July 2020).
2 Falco, Miriam, et al., American Cancer Society medical and editorial content team. “Ultraviolet (UV) Radiation: What is UV radiation?” American Cancer Society Inc., 10 July 2019, Available online: https://www.cancer.org/cancer/cancer-causes/radiation-exposure/uv-radiation.html (Accessed 28 May 2020).
3 Scientific Committee on Consumer Products, European Commission: Health & Consumer Protection Directorate-General. “Opinion on Biological Effects of Ultraviolet Radiation Relevant to Health with Particular Reference to Sunbeds for Cosmetic Purposes.” 20 June 2006, Available online: https://ec.europa.eu/health/ph_risk/committees/04_sccp/docs/sccp_o_031b.pdf (Accessed 28 May 2020).
4 Lindblad, M., Tano, E., et al., “Ultraviolet-C Decontamination of a Hospital Room: Amount of UV Light Needed.” Burns, Elsevier Ltd., 30 October 2019, Available online: https://doi.org/10.1016/j. burns.2019.10.004 (Accessed 28 May 2020).
5 National Research Council (US) Committee on Toxicology. Emergency and Continuous Exposure Limits for Selected Airborne Contaminants: Volume 1. Washington (DC): National Academies Press (US); 1984. OZONE. Available from: https://www.ncbi.nlm.nih.gov/books/NBK208281/
6 Bullard, Gabe, “Goodbye, Open Office? How Workspaces Will Change After Coronavirus.” WAMU, 19 May 2020, Available online: https://wamu.org/story/20/05/19/goodbye-open-office-how-workspaces-will-change-after-coronavirus/ (Accessed 28 May 2020).


